Liver Cirrhosis
Liver cirrhosis is a serious condition that affects the liver, one of the most vital organs in our bodies. It occurs when healthy liver tissue is replaced by scar tissue, preventing the liver from functioning properly. In this article, we will delve deeper into understanding liver cirrhosis, its causes and risk factors, the signs and symptoms you shouldn't ignore, how it is diagnosed, the various treatments available, and the potential complications that can arise from this condition.
Understanding Liver Cirrhosis: Causes and Risk Factors
Liver cirrhosis is often the result of long-term liver damage caused by factors such as excessive alcohol consumption, chronic viral hepatitis (such as hepatitis B or C), fatty liver disease, autoimmune diseases, and certain inherited disorders. Obesity, diabetes, and exposure to certain toxins can also increase the risk of developing cirrhosis.
While anyone can develop liver cirrhosis, certain factors can increase the chances. Age, gender (men are more susceptible), and genetic predisposition can contribute to the risk. Additionally, individuals who abuse drugs and alcohol, have unprotected sex ( sexually transmitted hepatitis B), or have previously had liver diseases are also more prone to developing cirrhosis.
It is important to note that liver cirrhosis is a progressive condition that can lead to serious complications if left untreated. As the liver becomes increasingly scarred and damaged, its ability to function properly diminishes. This can result in a variety of symptoms, including fatigue, jaundice, swelling in the legs and abdomen, easy bruising, and mental confusion.
Furthermore, individuals with liver cirrhosis are at an increased risk of developing liver cancer, as the damaged liver cells are more likely to undergo malignant transformation. Regular monitoring and screening for liver cancer are essential for early detection and treatment.
Signs and Symptoms of Liver Cirrhosis You Shouldn't Ignore
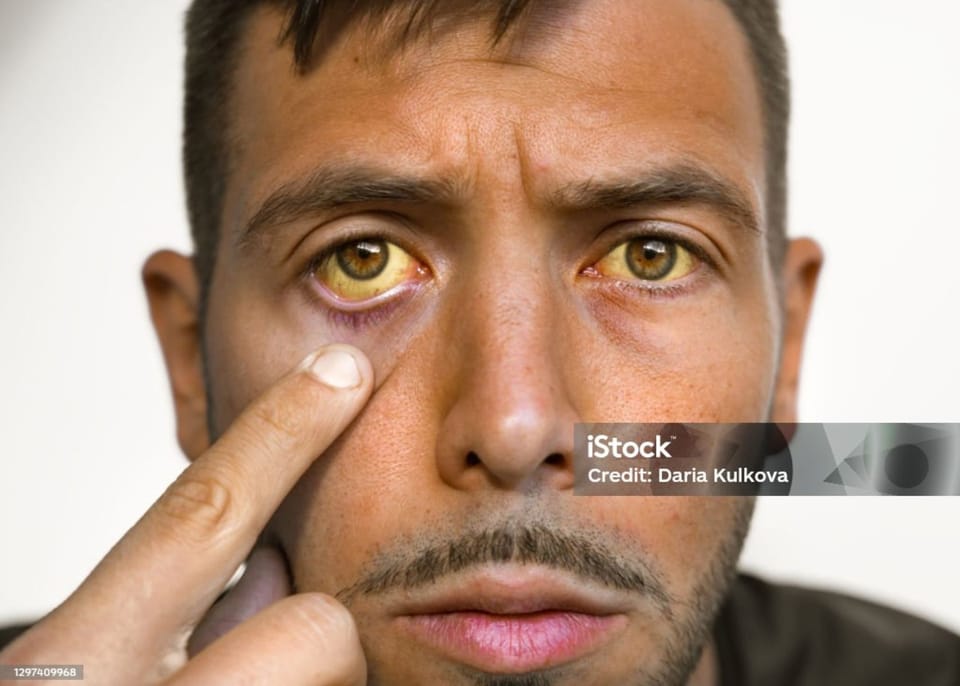
The early stages of liver cirrhosis may not present any noticeable symptoms. However, as the disease progresses, various signs and symptoms can arise. Some common symptoms include fatigue, weakness, yellowing of the skin and eyes (jaundice), itching, fluid retention (swelling in the legs and abdomen), weight loss, and easy bruising or bleeding.
It is important to pay attention to these symptoms and seek medical advice if they persist, as early detection and intervention can significantly improve outcomes and prevent further liver damage.
Furthermore, individuals with liver cirrhosis may also experience cognitive issues such as confusion, difficulty concentrating, and memory problems. This can be attributed to the liver's role in detoxifying harmful substances in the body, including those that affect brain function. Additionally, as cirrhosis progresses, complications such as portal hypertension may develop, leading to symptoms like enlarged veins in the esophagus (esophageal varices) and abdominal discomfort.
Diagnosing Liver Cirrhosis: Tests and Procedures
Diagnosing liver cirrhosis typically involves a combination of a medical history review, physical examination, and diagnostic tests. During the physical examination, your healthcare provider may look for signs such as an enlarged liver or spleen, jaundice, or fluid accumulation.
Further testing may include blood tests to measure liver function, imaging tests such as ultrasound or MRI, and liver biopsy to assess the extent of liver damage. These tests help confirm the diagnosis and determine the severity of the cirrhosis.
It's important to note that liver cirrhosis can be caused by various factors, including chronic alcohol abuse, viral hepatitis, and fatty liver disease. Understanding the underlying cause of cirrhosis is crucial for determining the most effective treatment plan and preventing further liver damage.

In addition to the diagnostic tests mentioned above, your healthcare provider may also recommend a transient elastography test, which measures liver stiffness to assess the degree of fibrosis present. This non-invasive procedure provides valuable information about the progression of cirrhosis and helps guide treatment decisions.
Treatments for Liver Cirrhosis: Medications and Lifestyle Changes
While there is no cure for liver cirrhosis, treatment focuses on managing symptoms, preventing complications, and slowing down the progression of the disease. Lifestyle changes play a crucial role, including maintaining a healthy diet, abstaining from alcohol, and controlling other underlying conditions such as diabetes or obesity.
In some cases, medications may be prescribed to manage specific symptoms or complications. For example, diuretics may be given to reduce fluid retention, while antiviral medications can help control viral hepatitis. In advanced cases, a liver transplant may be the only option to restore liver function.
Individuals with liver cirrhosis need to work closely with their healthcare team to monitor the progression of the disease and adjust treatment plans as needed. Regular check-ups, blood tests, and imaging studies can help track liver function and detect any complications early on. Additionally, support groups and counseling services can provide emotional support and guidance for both patients and their families as they navigate the challenges of living with liver cirrhosis.
Furthermore, incorporating regular exercise into a daily routine can help improve the overall health and well-being of individuals with liver cirrhosis. Physical activity can aid in weight management, reduce the risk of developing fatty liver disease, and improve cardiovascular health. Engaging in activities such as walking, swimming, or yoga can also help reduce stress levels and promote mental clarity.
Complications of Liver Cirrhosis: What You Need to Know
Unfortunately, liver cirrhosis can lead to various complications that can be life-threatening if not properly managed. These complications include portal hypertension (high blood pressure in the vein that carries blood to the liver), liver cancer, kidney failure, and hepatic encephalopathy (a decline in brain function).
To minimize these risks, it is crucial to follow a comprehensive treatment plan, adhere to prescribed medications, and regularly monitor liver function through scheduled checkups and tests. Timely intervention and close medical supervision can help prevent or effectively manage these complications.
Portal hypertension, a common complication of liver cirrhosis, can lead to the development of varices, which are enlarged, swollen veins in the esophagus or stomach. These varices are at risk of rupturing, causing severe bleeding that can be life-threatening. Patients with liver cirrhosis and portal hypertension may require procedures such as endoscopic band ligation or transjugular intrahepatic portosystemic shunt (TIPS) to prevent variceal bleeding.
Liver cancer, also known as hepatocellular carcinoma, is another serious complication that can arise in patients with liver cirrhosis. Regular surveillance with imaging studies such as ultrasounds or MRIs is essential for early detection of liver cancer in high-risk individuals. Treatment options for liver cancer may include surgery, liver transplant, chemotherapy, or radiofrequency ablation, depending on the stage of the cancer and the patient's overall health.
Thanks for reading.
BestPharmaReviews.



